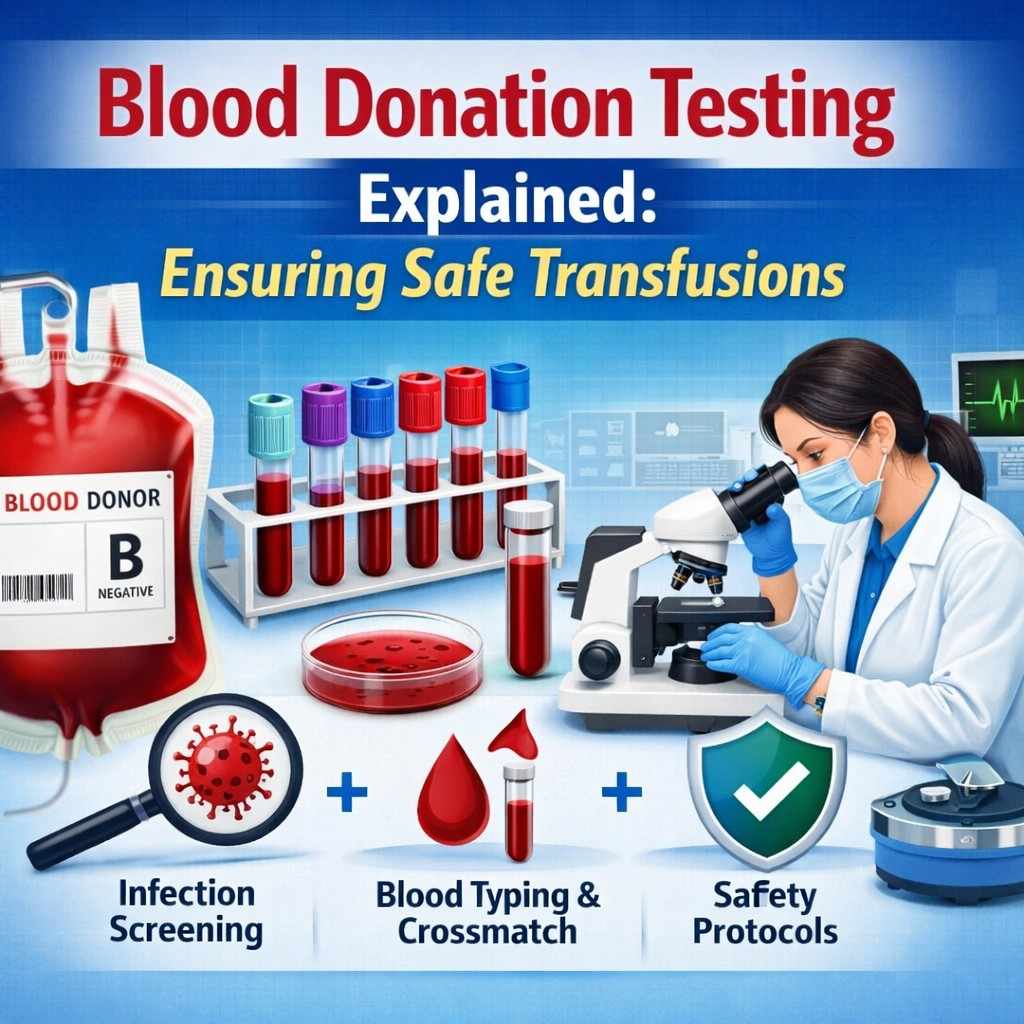
Blood transfusion is a life-saving medical procedure used in surgeries, trauma care, childbirth complications, cancer treatment, and chronic blood disorders. To ensure patient safety, every unit of donated blood goes through a strict and multi-layered testing process before it is approved for transfusion. These safety protocols are designed to prevent infections, ensure compatibility, and maintain the highest standards of medical care.
1. Donor Screening Before Blood Collection
Safety begins even before blood is drawn. Potential donors are carefully screened through a questionnaire and basic health checks. This includes questions about medical history, recent illnesses, travel history, medications, and lifestyle factors that could increase infection risk. Vital signs such as hemoglobin levels, blood pressure, pulse, and body temperature are also checked. Only donors who meet all eligibility criteria are allowed to donate.
2. Blood Grouping and Typing
Once blood is collected, the first laboratory step is determining the blood group. Each unit is tested for ABO blood type (A, B, AB, or O) and Rh factor (positive or negative). Accurate blood typing is critical because transfusing incompatible blood can cause severe, sometimes fatal, reactions. This step ensures the right blood reaches the right patient.
3. Testing for Infectious Diseases
To prevent transfusion-transmitted infections, donated blood undergoes mandatory testing for several infectious diseases. These tests are performed using advanced laboratory techniques to detect even early-stage infections. Commonly tested infections include:
-
HIV (Human Immunodeficiency Virus)
-
Hepatitis B
-
Hepatitis C
-
Syphilis
-
Malaria (especially in regions where it is prevalent)
If any test result is positive, the blood unit is immediately discarded and never used for transfusion.
4. Antibody Screening
In addition to blood grouping, laboratories perform antibody screening to detect unexpected antibodies in the donor’s blood. These antibodies can develop due to previous transfusions or pregnancies. If present, they may cause complications during transfusion. Identifying these antibodies helps blood banks select the safest possible match for patients.
5. Crossmatching Before Transfusion
Before blood is transfused to a patient, a crossmatch test is performed. This involves mixing a small sample of the patient’s blood with the donor blood to check for any adverse reaction. Crossmatching ensures complete compatibility and reduces the risk of transfusion reactions such as hemolysis or allergic responses.
6. Component Separation and Storage
After testing, whole blood is usually separated into components such as red blood cells, plasma, and platelets. Each component is stored under specific temperature-controlled conditions to preserve quality and safety. Blood banks strictly monitor storage duration and conditions to prevent contamination and degradation.
7. Quality Control and Documentation
Blood banks follow national and international regulatory standards to maintain safety. Every step—from donor screening to testing and storage—is documented and audited. Regular quality checks, equipment calibration, and staff training ensure that protocols are followed without compromise.
8. Final Verification Before Use
Before transfusion, healthcare professionals recheck blood labels, patient identity, and compatibility reports. This final verification step acts as an additional safety barrier to eliminate human error.
Why These Protocols Matter
These comprehensive testing and safety measures make modern blood transfusion extremely safe. The risk of contracting infections from transfused blood is now very low due to advancements in testing technology and strict regulations. Patients can receive blood with confidence, knowing that multiple safeguards are in place.
Conclusion
Blood testing before transfusion is a critical process that protects both patients and healthcare systems. From donor screening to advanced laboratory testing and final verification, every step is designed to ensure safety and reliability. This rigorous process highlights the importance of voluntary blood donation and the role of blood banks in saving lives safely and responsibly. Momodo sex nude gif