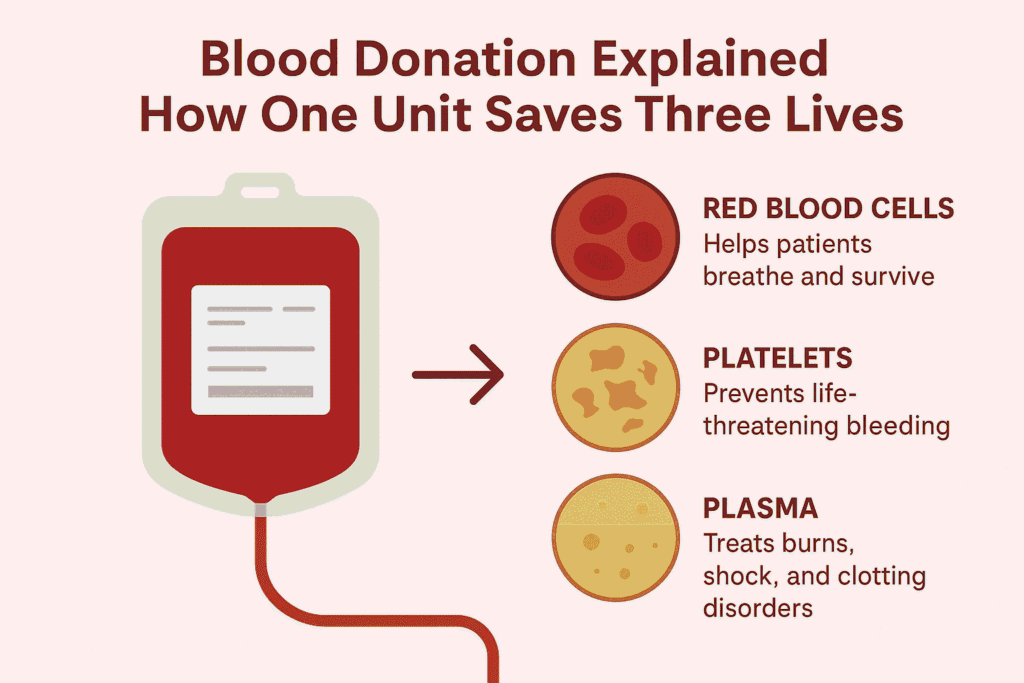
Blood donation is one of the most powerful acts of humanity—simple, quick, and lifesaving. You may have often heard the phrase “One unit of blood can save three lives.” But how is this possible? Understanding what happens after blood is donated helps us realize why every drop matters and why regular blood donation is so important.
What Is One Unit of Blood?
When a person donates blood, approximately 350–450 ml (about one unit) of whole blood is collected. This donation is safe for a healthy adult, and the body naturally replenishes the donated blood within a few weeks. What makes this act extraordinary is that this single unit is not used as-is for only one patient—it is carefully processed and divided into multiple components.
Separation of Blood Components
After donation, the collected blood is sent to a blood bank or processing center. Here, it is separated into three main components using specialized equipment:
-
Red Blood Cells (RBCs)
-
Platelets
-
Plasma
Each component serves a unique medical purpose and can be given to different patients. This is how one unit of blood can potentially help three different people, each with different medical needs.
How Each Component Saves Lives
1. Red Blood Cells – Helping Patients Breathe and Survive
Red blood cells are responsible for carrying oxygen from the lungs to the rest of the body. Patients who suffer from:
-
Severe blood loss due to accidents or surgeries
-
Anemia
-
Childbirth-related complications
-
Major trauma
often require RBC transfusions. One unit of donated blood can provide enough red blood cells to stabilize a patient in critical condition and help restore oxygen levels in the body.
2. Platelets – Lifesaving for Cancer and Critical Patients
Platelets help the blood clot and prevent excessive bleeding. They are especially vital for:
-
Cancer patients undergoing chemotherapy
-
Leukemia patients
-
Dengue and viral fever patients
-
Those with severe bleeding disorders
Platelets have a very short shelf life (usually 5–7 days), which makes regular blood donation essential. Platelet transfusions can prevent life-threatening bleeding and help patients recover safely.
3. Plasma – Treating Burns, Shock, and Clotting Disorders
Plasma is the liquid portion of blood that carries proteins, hormones, and clotting factors. Plasma transfusions are commonly used for:
-
Burn victims
-
Patients in shock
-
Liver disease patients
-
People with clotting disorders such as hemophilia
Plasma plays a crucial role in maintaining blood pressure, volume, and proper clotting—often making the difference between life and death in emergencies.
Beyond Three Lives: Even Greater Impact
In some cases, blood components can be further processed into specialized products like:
-
Cryoprecipitate (for clotting factor deficiencies)
-
Plasma-derived therapies
This means a single donation may indirectly help even more than three patients, especially in large hospitals and trauma centers.
Why Regular Blood Donation Matters
The demand for blood is constant. Road accidents, surgeries, cancer treatments, childbirth complications, and medical emergencies happen every day. Blood cannot be manufactured—it can only come from generous donors.
Regular voluntary donation ensures:
-
A stable blood supply
-
Availability of different blood groups
-
Emergency readiness
-
Reduced dependency on replacement donors
A Small Act with a Massive Impact
Donating blood takes about 10–15 minutes, but its impact can last a lifetime for someone in need. The phrase “one unit of blood can save three lives” is not just a slogan—it is a medical reality backed by science and daily hospital practices.
By choosing to donate blood, you are choosing to give hope, health, and life. A single act of kindness can turn into three second chances at life.